Starting on Opioids
Prescribing opioids to manage pain is a common practice in Ontario and across North America. Canadians are the second largest per-capita users of prescription opioids after the U.S. at over 34,000 daily doses (equivalent to 100 mg of morphine) per million people in 2013-2015, compared to 12,000 daily doses per million in the U.K., 10,000 in Sweden, and 1,200 in Japan.[1]
In Ontario, “new starts” of opioids – that is, prescriptions of opioids for people who have not filled an opioid prescription in the last six months – accounted for about 15% of all opioid prescriptions in 2016, or about 1.3 million out of 8.3 million (excluding prescriptions for people receiving palliative care, and prescriptions for cough medication that contains opioids). Many of these opioids were likely newly prescribed to treat acute pain for things like broken bones, pain after surgery, and dental pain, but they could also have been prescribed for other reasons, including initiating or restarting opioids for chronic pain.
Why focus on new starts?
New evidence on opioids contributed to the recommendations in the 2017 opioids guidelines for chronic non-cancer pain in Canada.[2] Health Quality Ontario followed up with three forthcoming quality standards – concise sets of statements, based on the best available evidence, outlining what care should look like for patients with certain conditions – for opioid prescribing in Ontario. These standards, for acute pain, chronic pain, and opioid use disorder, are aligned with the Canadian guidelines.[3]
The guidelines and quality standards both highlight new starts to improve prescribing practices. This report focuses on new starts of opioids so that prescribers and patients can reflect on whether there are non-opioid treatments, lower dosages or durations they should consider when starting on opioids to prevent long-term use, which can lead to significant harm.[4]
Prescriptions for people who are already taking opioids – typically for ongoing pain – have their own important concerns that deserve further study.
More opioid prescriptions for smaller amounts of opioids could be a good sign
About one in seven people in Ontario, or 1.6 million people, filled at least one prescription for an opioid in 2016. The total number of opioid prescriptions filled increased to almost 8.3 million in Ontario (excluding prescriptions for cough and for palliative care), up by more than 500,000 prescriptions filled over the last three years.
But according to a recent Ontario Drug Policy Research Network report, this increase may be a sign that prescribers are being more cautious in their prescribing, by writing more prescriptions but for a shorter average duration.[5] Prescribing for a shorter duration is important as prescriptions of less than seven days’ worth of opioids may reduce the likelihood of continued use and harms.[6]
Balancing potential benefits and harms
In some cases, opioids are the best treatment option. Opioids play an important role, in particular, in pain management for people receiving palliative care. People should discuss with their doctor, surgeon, nurse practitioner, or dentist, a pain management strategy that’s right for them. However, our knowledge about the potential harms from opioids has increased considerably in recent years. Many people who are prescribed opioids experience side effects, and some people develop an opioid use disorder (problematic use of opioids that causes significant impairment or distress).
Most importantly, opioid toxicity is an increasingly common cause of death. In 2016, 867 people in Ontario died from opioid toxicity, up from 366 in 2003.[7] And, opioid-related emergency department visits more than doubled to 4,427 in 2016 from 1,858 in 2003.[8] While many deaths involve opioids that were obtained from street sources, patients treated by doctors who prescribe opioids frequently account for a much higher proportion of opioid-related deaths than patients treated by doctors who prescribe opioids less often.[9] Careful prescribing of opioids is only one aspect of addressing this complex issue. Other aspects include better identification and treatment of opioid use disorder, harm reduction and overdose prevention, and improved access to other treatments for pain.
Prescriptions – what we looked at
The data on new starts reported here – prescriptions for people who have not filled an opioid prescription in the last six months – come from the Narcotics Monitoring System, which collects information on opioid prescriptions filled at Ontario pharmacies. It does not include prescriptions filled in hospitals or prisons, nor does it collect information on street sources of opioids.
Health Quality Ontario excluded prescriptions for methadone and buprenorphine/naloxone – opioids that are used to treat opioid use disorder – as well as those for cough, and for palliative care. These are also excluded from the main recommendations in the forthcoming quality standards for opioid prescribing for acute and chronic pain.
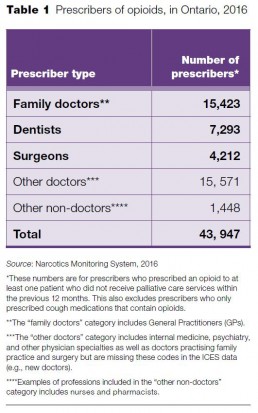
Who prescribes opioids in Ontario?
About 44,000 health care professionals in Ontario prescribed opioids in 2016. We examined new starts of opioids by the three groups who prescribed the largest share of all new starts of opioids: family doctors, surgeons, and dentists. Together, these three groups represented 86% of all new start prescriptions in 2016.
The family doctors group includes doctors who identified family practice as their main specialty. Within the family doctors group, there is variation in the scope of practice, but this report does not examine how prescribing patterns might differ by practice type. Types of practice include general practitioners (GPs), doctors who are providing primary care to a broad group of patients, but also family doctors who are providing focused care in areas such as emergency medicine, anesthesia, pediatrics, geriatrics, and sports medicine.
“Other doctors” includes a variety of specialties, such as internal medicine and psychiatry, where either the number of providers in the specialty or the volume of opioid prescribing was too small to be able to report individually in a meaningful way. This category also includes doctors who were missing information on specialty, possibly because they had not yet declared their specialty. It’s possible that a small number of family doctors and surgeons are included in this group.
Opioid prescribing patterns in emergency departments are an area of significant concern. However, we are unable to accurately report on these patterns with the current data, since many emergency department doctors list their primary specialty in other areas, such as family medicine. Work is underway to improve the use of the available data to understand more about opioid prescribing in the emergency department.
Nurse practitioners, included in the “other non-doctors” group, accounted for about 2% of the total prescribers (or 938) in 2016, and they were only authorized to prescribe tramadol and tapentadol. The number of nurse practitioners who prescribe opioids will likely rise in the near future as prescribing practice standards for nurse practitioners were expanded in 2017 to include all opioids.[10]
Prescriber numbers, at a glance
Of the almost 1.3 million new starts of opioids in Ontario in 2016, family doctors prescribed almost half of them, surgeons prescribed about one-fifth and dentists less than one-fifth. Looking at the proportion of each provider type’s opioid prescriptions that were new starts, about 1 in 10 of family doctors’ opioid prescriptions for opioids in 2016 were new starts, while more than half of surgeons’ opioid prescriptions were new starts, and nearly three-quarters of dentists’ opioid prescriptions were new starts.
Four areas of focus
To gain insight into the new starts of opioid prescriptions in Ontario, we look at the prescribing practices of family doctors, surgeons and dentists, focusing on areas of potential improvement, based on the evidence:
1. New starts of opioids, trend over time
2. Starting on high doses of opioids (over 90 mg of morphine equivalent)
3. New starts of hydromorphone and tramadol
4. Starting with a supply of more than 7 days’ worth of opioids
We also look at variation by Local Health Integration Network (LHIN) region, when notable.
1. There were nearly 1.3 million new starts of opioid prescriptions in Ontario in 2016
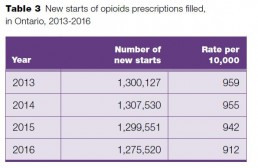
New starts of opioids decreased slightly in 2016 from 2013, by about 25,000, or 2%.
Of the almost 8.3 million non-palliative care opioid prescriptions filled in 2016, almost 1.3 million (about 1 in 6) were for people who had not filled an opioid prescription written by an Ontario prescriber in the previous six months.
New starts of opioids decreased to 1,275,520 in 2016 from 1,300,127 in 2013, and the rate of new starts per 10,000 population also decreased to 912 per 10,000 people in 2016 from 959 per 10,000 people in 2013.
Falling and rising
Sara, a university student in Vaughan, tells the story of her journey of pain, the stigma of opioids, and the road back to school and friends
It was just a regular softball practice. Standing near second base, Sara, who was 15 at the time, watched her teammate hit a hard line drive, and before she could get her glove up, the ball flew directly into her left eye socket. She didn’t even have time to close her eye. At the hospital, doctors told Sara she had major damage to her eye, and a series of fractures to her orbital socket and along the upper left side of her face.
The first start
The fractures were healing on top of the nerve, causing pain that radiated from under her eye, into her jaw, ear, and scalp. She took Tylenol 3, which contains the opioid codeine, in the hospital that night, and was prescribed seven days worth of Tylenol 3 from the emergency department doctor. “I guess they weren’t comfortable with prescribing for more than that,” she says. The fractures were expected to take six weeks to heal completely. “Because of that,” Sara says, “they said I could just take Advil. I started taking extreme amounts of Advil and ended up getting an ulcer.”
About six months later, Sara had ongoing pain from her injury, and went to a pain clinic in Toronto, where doctors tried different medications, including nerve medications, nonsteroidal anti-inflammatory drugs (NSAIDs), and opioids. “At that point, my parents and my doctors gave me very firm warnings about the paths you could go down by getting addicted to opioids,” Sara says. “At first, taking opioids felt like a failure, like I’m not able to handle my pain well enough.” Since this injury was mostly nerve pain, Sara says she never really found relief from the opioids, so the doctors decided it wasn’t worth it to continue on them.
Surgery
In 2011, Sara had surgery to remove the bone fragments that were compressing the nerve above her eye. She was given the opioid hydromorphone in hospital to manage the pain. “I had a really, really intense pain coming out of that surgery,” she says. Sara left the hospital with a prescription for a few days’ worth of hydromorphone.
Three years later, in 2014, Sara was prescribed opioids after surgery to remove a benign tumour near her eye, which was causing her a lot of pain. That time, she took hydromorphone tablets for about six weeks, prescribed first by the surgeon for two weeks, and then by the doctor at the hospital pain clinic. She followed a schedule to carefully decrease her daily dose, near the end of the prescription. She briefly took opioids shortly afterward, after getting four fillings at the dentist, which flared up the pain in her face from the softball injury. The dentist prescribed her Tylenol 3 for a few days.
The fall
The next year, in 2015, Sara slipped and fell during a hike, severely injuring her lower back. The emergency department doctor wrote her a prescription for a few days’ worth of Percocet, which contains the opioid oxycodone. After the initial pain from the injury, Sara kept reaggravating her back every four or five months. “All I had to do was lift my bag and it would give me a pain flare that would have me lying flat on my back,” she says.
The pain, Sara says, took hold in different ways. She had constant nerve pain down her legs, feet and toes, which felt like a deep tightness. Her legs would go numb sometimes. And then there was a deep pain in her bones that “felt like somebody was hammering my back at every step.” After two years of on-and-off pain, Sara had spinal surgery in the summer of 2017. She awoke after the surgery in extreme pain and was given a few different opioids while in hospital.
When she left the hospital, Sara was given a prescription for two days’ worth of opioids. “From there, we had to make an emergency visit to my family doctor’s clinic and ask her to help us with pain medication and management to make it through to our pain clinic appointment,” Sara says. “It was a very, very rough time. My pain was very out of control. It was basically like blackout pain. It was just a nightmare.”
Through the pain clinic at the hospital, Sara was prescribed opioids, but also had access to a physiotherapist and a psychologist, which together allowed her to regain the three things she was struggling with: mobility, pain, and emotions. “Stress and anxiety can worsen pain,” Sara says. “It’s really easy to get depressed in these situations. Every day, I try to stay positive. Although I fell down so far, I’m also coming back up.” Sara, who was in a wheelchair after the surgery, wondered if she would ever walk again.
Rising
When she was eventually able to walk 10 steps, Sara realized how far down she had fallen from her previously active self. She thought about how she had to leave school, which was a big part of her identity, and about the friendships she had lost. “I went from driving myself wherever I wanted and working and feeling capable and intelligent to feeling slow and confused. Everyone else was continuing with their lives and I was on pause.”
Sara’s condition improved, and she has now reduced the amount of opioids she takes. “I’m working very hard on non-pharmaceutical solutions to what I’m going through. I’m getting better, and I’m so thankful for that. My family has been so amazing throughout this whole thing. I’m so thankful for them, so I try my best to be positive.” Sara’s goal for the future is to stop taking opioids completely.
Helping
There is a stigma associated with opioids, Sara says, especially as a young person. “All we’re trying to do is cope with pain,” she says. Everywhere Sara turned, she faced questions about why she needed the medication, and about the doses. “There had to be some doctor willing to stick their neck out for you to give you an opioid prescription,” Sara says.
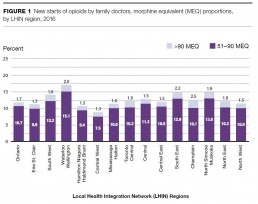
2. High-dose new starts of opioids by surgeons vary widely by LHIN region
Regional variation in the proportion of new starts by surgeons with doses over 90 mg of morphine equivalent (MEQ) in 2016 ranged from 3.0% in the North West LHIN region to 11.8% in the Champlain LHIN region. There was also some LHIN region variation among family doctors and dentists.
About 3.4%, or 42,111, of the total new starts in Ontario in 2016 were for over 90 MEQ, and 16%, or 197,169, were for doses of 51–90 MEQ.
Why high-dose new starts matter
Starting someone on a dose of opioids higher than 90 MEQ has been shown to increase the risk of death from opioid poisoning relative to starting on a low dose. Starting on a dose over 50 MEQ also increases the risk of death relative to a low dose.[11]
Family doctors
Among the new starts of opioid prescriptions by family doctors in 2016, 9,704 (or 1.7%) were above 90 MEQ. This declined from just over 12,556, or 2.0% of the total, in 2013.
There were 61,706, or 10.7% of new starts with a dose from 51–90 MEQ by family doctors in 2016. These also decreased from 76,740, or 12.1% of the total, in 2013.
There is some variation by LHIN region for the percentage of new starts above 90 MEQ by family doctors in 2016, ranging from a low of 1.3% in the Erie St. Clair, Hamilton Niagara Haldimand Brant and Central West LHIN regions to a high of 2.5% in Champlain LHIN region. LHIN region variation for new starts of 51–90 MEQ ranged from a low of 7.5% in Central West LHIN region to a high of 15.1% in Waterloo Wellington LHIN region.
Surgeons
Among the new starts of opioid prescriptions by surgeons in 2016, 21,297 (or 8.0%) were above 90 MEQ. This increased from 19,956, or 7.1% of new starts in 2013.
There were 74,318 new starts with doses from 51–90 MEQ by surgeons in 2016, down from 80,092 in 2013, while the proportion of new starts with doses from 51–90 MEQ remained consistent between 2013 and 2016 at approximately 28.0%.
Variation by LHIN region for the proportion of new starts with doses over 90 MEQ in 2016 ranged from 3.0% in the North West LHIN region to 11.8% in the Champlain LHIN region. For doses from 51–90 MEQ, variation ranged from 18.0% in the North West LHIN region to 34.1% in the Waterloo Wellington LHIN region.
Dentists
There were relatively few new starts of opioids above 90 MEQ prescribed by dentists – 1,515 in 2016, down from 1,995 in 2013, making up just 0.7% of total new starts among dentists.
There were, however, 24,215 new starts from 51–90 MEQ by dentists in 2016, making up 11.0% of dentists’ new starts, down from 26,256 or 11.9%, in 2013.
Variation by LHIN region for the proportion of new starts with doses over 90 MEQ in 2016 ranged from 0.2% in the North West LHIN region to 1.6% in the Champlain LHIN region. For doses from 51–90 MEQ, variation ranged from 7.4% in the North West LHIN region to 15.4% in the Champlain LHIN region.
Managing pain
Dr. Hance Clarke, director of a transitional pain program at a hospital in Toronto, describes some strategies for pain management and opioid prescribing
Three types of responses
“You get one of three reactions to an opioid: ‘It’s gross, it makes me sick, and I vomit,’ or ‘it reduces my pain, it’s a good choice.’ And then you get, ‘this feels amazing,’ and for this group, even for the low doses, it is sometimes hard for many of them to stop. You’re starting to see prescribers develop a strategy to know who is at risk in that third group. Does your patient have a history of anxiety or depression? How many drinks do they have per week? How intense is their pain? How much does the pain interfere with their life? Prescribers need to understand the subset of the population who is at risk for inappropriately persisting on their opioid medication, and those for whom the opioid provides benefit.”
“How easy is it for the people in the first two groups to stop taking opioids? It is usually dose-dependent. We do a good job of prescribing, but not as good of a job describing and managing the potential consequences.”
Starting on opioids
“When it comes to the family physician, based on the data, it appears as though we have developed a practice where we sometimes treat chronic [long-lasting] pain the way we treat acute [sudden] pain. I think primary care doctors should do their best to move away from the prescribing of opioids for chronic pain as a first-line treatment. By using guidelines such as the Canadian Pain Society neuropathic pain guidelines, patients can be started on other classes of drugs, and move the opioid medication into the background. The need for the opioid can be reassessed based on the patient’s response.”
“Looking at the variation and complexity of surgical interventions, there is a wide variation in postoperative prescribing practices by surgeons. Some surgeons prescribe only Tylenol 3 [containing the opioid codeine] and others send patients home with prescriptions of hydromorphone.
From a harm reduction standpoint, there are grounds to question these practices. Perhaps it’s best to discharge patients with a less potent opioid when clinically appropriate.”
“From the dentists’ and dental surgeons’ perspective, other than after maxillofacial surgery [such as surgery for a broken jaw] or facial reconstruction, is there a need to prescribe opioids?
There are very effective and potent anti-inflammatory medications in conjunction with acetaminophen that can be used to manage pain effectively after tooth extractions and root canals. Use of opioids in these situations should be avoided if at all possible.”
A plan to stop
“An informed discussion regarding the risks of opioids, as well as how to wean off your medication, should be had at the outset of prescribing opioids. The rare but most serious complication is that you might die from respiratory depression. After that, it’s that you’re going to develop physiological tolerance and stay on them long-term. When you start on opioids, you need to know how to stop. Even if you’re on an opioid for two weeks, you might experience some withdrawal symptoms when stopping.”
Other options
“When it comes to the treatment of chronic pain conditions, we must ensure that we start with non-pharmacological and non-opioid medication options before we jump to an opioid medication. The options are many – massage, physiotherapy, ice, heat, acetaminophen, muscle relaxants, anti-convulsants, antidepressants, cannabinoids – there’s a whole host of possibilities, some are covered by the government currently, while others are not. Most importantly, let’s not forget to mention the psychological impact on people suffering with chronic pain, and the role of psychotherapy and mental health interventions. Patients often discover that once they add several non-opioid options, they gain even more control over their pain and improve their quality of life.”
3. New starts of hydromorphone and tramadol are increasing
New starts of hydromorphone by family doctors increased to over 60,000 in 2016 from about 41,000 in 2013, and by surgeons to nearly 34,000 in 2016 from about 26,000 in 2013. Tramadol also increased, while new starts for most of the other opioid types were down or mostly unchanged.
The proportion of new starts of hydromorphone and tramadol increased between 2013 and 2016, two of the only types of opioids with a notable increase. We don’t know the exact reasons for these increases of new starts, but hydromorphone has become a more favoured opioid over oxycodone since OxyContin was delisted from Ontario’s drug benefit program in 2012.[12] The increase in tramadol prescribing is associated with it being marketed as a non-opioid, and as being less addictive.[13] But Health Canada has launched a review of scientific evidence to consider whether to classify it as an opioid under the Controlled Drugs and Substances Act.[14]
Hydromorphone is a strong opioid, five times more potent than morphine. By comparison, oxycodone is 1.5 times stronger than morphine.[15]
Tramadol is metabolized differently from person to person, and among opioids, has a unique set of potential harms, including an increased risk of hypoglycemia ( low blood sugar ) and seizures.[16,17,18]
Family doctors
Hydromorphone accounted for about 60,000, or 10.0%, of new starts of opioids by family doctors in 2016, which increased from 41,000, or 6.2%, of new starts from 2013 – the only opioid type that experienced this level of growth.
Similarly, there were more than 60,000 new starts of tramadol by family doctors in 2016, 10.3% of their total new starts of opioids, up from just over 55,000, or 8.4%, of new starts in 2013.
There is substantial LHIN region variation in the rate of new starts of hydromorphone by family doctors, ranging from 26.1 per 10,000 population in the Mississauga Halton LHIN region to 86.5 per 10,000 population in the Champlain LHIN region in 2016.
There is also substantial LHIN region variation in the rate of new starts of tramadol by family doctors, ranging from 13.7 per 10,000 population in the Toronto Central LHIN region to 121.8 per 10,000 population in the Erie St. Clair LHIN region in 2016.
Surgeons
Hydromorphone accounted for about 34,000, or 12.2%, of new starts of opioids by surgeons in 2016, up from about 26,000, or about 9.0%, of new starts in 2013.
Tramadol accounted for nearly 34,000, or 12.2%, of new starts of opioids by surgeons in 2016, up from about 26,000, or 9.1%, of new starts in 2013.
There was minimal LHIN regional variation for new starts of hydromorphone and tramadol by surgeons.
Dentists
Hydromorphone accounted for just over 1,600, or 0.7%, of new starts of opioids by dentists in 2016, up from about 700, or 0.3%, of new starts in 2013.
There were over 7,000 new starts of tramadol by dentists in 2016, 3.2% of the total new starts by dentists, up from more than 6,000, or 2.8% of new starts in 2013.
Codeine combination opioids, such as Tylenol 3, accounted for 80.0% of new starts of opioids by dentists in 2016, and that trend is consistent.
There was minimal LHIN regional variation for new starts of hydromorphone and tramadol by dentists.
From doctor to patient
Sheldon, a medical oncologist in Mississauga, tells his story as a patient, who was prescribed opioids after a major lung surgery
“It began last year when I was walking the dog. It was Boxing Day. I slipped on black ice and fell hard. I went back to work, but the pain wasn’t getting any better, so I went in for an X-ray. They confirmed that I had fractured one of the vertebrae in my spine. But what they also saw was a very large mass in the right upper lobe of my lung. It had essentially occupied half of my lung, and had pushed my heart over to one side. The panic that ensues when you know what it might be was pretty intense.”
“I had no symptoms from it because I had run a half-marathon three weeks before, and skied two weeks before. The thoracic surgeon organized a biopsy, which confirmed that this was a benign type of tumour, but it was compressing my heart and other things, so it needed to come out. It was 16 centimetres. If I had let it go another centimetre, I would’ve had the largest one ever [at that hospital].”
A pain crisis
“The surgery was long and complicated – a nine-hour procedure. I lost 13 units of blood. The recovery in hospital was relatively easy. I was in for three days. The problem was when I went home, within 48 hours, I was in a terrible pain crisis. They had to cut into my neck to get the tumour out, so I was having terrible arm pain. There was also a burning pain, like someone scalded my skin. At that time, I was on 30 milligrams a day of the opioid hydromorphone, and that just wasn’t cutting it.”
“I had a good family doctor, and spoke with him and with the surgical team, and between the two of them they agreed to adjust the medication. It was escalated, but it didn’t really have much effect on relieving the pain. What it did produce was tiredness, and severe constipation – a terrible side effect of opioids.”
“I went to that emerg, and they suggested that I see the pain management team. In that visit, we came up with a plan, which was to provide adequate opioids, but supplement that with medication which would relieve some of the neuropathic [nerve] pain, and also begin to cut down on some of the anxiety, because the more pain you get, the more anxious you get. At my peak when I was unwell, I was on 120 milligrams a day of hydromorphone, which even for my practice in cancer care is a pretty big dose.”
Reducing the dose
“The major challenges in reducing pain meds don’t happen immediately, but as you get down to almost nothing you get problems with withdrawal. I knew what to expect, but it didn’t make it any easier. You feel fluey. You feel hot and cold, tired and shaky. There are medications that can help with some of those effects and they work pretty well. But I also had the commitment to myself and my family that drugs alone cannot make you better. You don’t always need a doctor – what you need is knowledge and understanding about the problem.”
“In time, and with some physio and mindfulness training, I was able to gradually get the dose down. My goal was really threefold: I wanted to restore my health, I needed to get back to work because I needed some purpose in what I was doing, and I needed to be more like the family person I was before. When you lose control and you’re not who you are, it’s very disturbing. We began reducing the doses of the opioids, in a scheduled and logical fashion. Over a period of the next three or four months, I was able to get off all opioids. I still take Tylenol. I went back to work full-time and competed in a marathon with two of my daughters.”
More than medication
“Getting the right care by the right team, and having strong family support, all of those components are important. What you do not want to do is rely on medication only. It doesn’t work. It has long-term potential serious side effects and you don’t need it. What you do need are alternative strategies. I’m very lucky, I didn’t have a malignant tumour. But I know there are a lot of people who have extensive surgery like I had who have a tough time getting off pain meds, and that’s a tragedy of our system, because it doesn’t have to be that way.”
“Before I had the surgery, I thought, I’d have the diagnostics and then the surgery, and the rest is kind of icing. I learned that’s not the case. Pain and symptom management are an essential component of major surgery. Full stop. When you haven’t gone through that, you don’t really appreciate it. The alternative is you would probably end up on opioids forever, and that’s not acceptable.”
“I’m not perfect now, but I come to work every day, and I’m happy that I’m able to do more of the things that I was doing before. My daughters and I are doing another run together, a half-marathon in Key West in January. Will I ever be 100%? Maybe not, but that’s OK, too. My only regret is that I asked for my specimen as a paperweight and I couldn’t get it.”
4. Nearly half of new starts of opioids by family doctors, and more than 1 in 10 new starts by surgeons, were for a supply of more than 7 days
There were 252,681 new starts of opioids by family doctors, and 32,077 new starts of opioids by surgeons for a supply of more than 7 days.
Why does a new start of opioids for a supply of more than 7 days matter?
A prescription for three days’ worth of opioids or less is often enough, and more than 7 days is indicated only in special circumstances, according to expert opinion,[19] which aligns with the forthcoming quality standard on opioids for acute pain. People who take opioids for more than 7 days are much more likely to become physically dependent and to experience withdrawal symptoms. Longer prescriptions that go unused may also end up being taken by family members, or others in the community without a prescription.[20]
Family doctors
There were more than 250,000 new starts of opioids with a supply of over 7 days prescribed by family doctors in 2016, accounting for 42.1% of the total new starts by family doctors. These numbers and proportions have changed little since 2013.
There was regional variation in the proportion of new starts by family doctors of opioids with a supply of over 7 days, ranging from a low of 35.9% in the North West LHIN region to a high of 48.6% in the Erie St. Clair LHIN region.
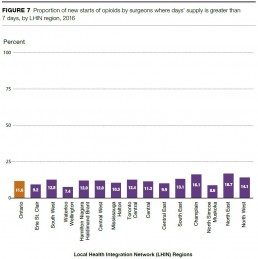
Surgeons
There were 32,077 new starts of opioids by surgeons for a supply of over 7 days in 2016, or 11.6% of the total new starts of opioids by surgeons. These numbers and proportions have changed little since 2013.
LHIN region variation in 2016 for new starts of opioids by surgeons for a supply of over 7 days ranged from a low of 7.4% in the Waterloo Wellington LHIN region to a high of 16.7% in the North East LHIN region.
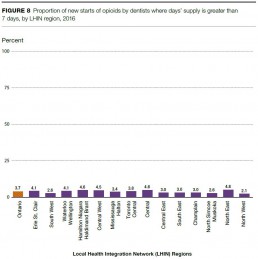
Dentists
Dentists prescribed relatively few new starts of opioids over 7 days’ supply, with just over 8,200 in 2016, or 3.7% of the dentists’ total new starts. These numbers and proportions have changed little since 2013.
LHIN region variation in 2016 for new starts of opioids by dentists for a supply of over 7 days ranged from a low of 2.1% in the North West LHIN region to a high of 4.8% in the North East LHIN region.
The patient first
Dr. Frank Warsh, a family doctor in London, shares his thoughts on starting patients on opioids
When starting a patient on opioids, Dr. Frank Warsh always keeps three things in mind: the patient’s preferences, the opioid prescribing guidelines, and the patient’s own body.
Every patient is different, and there’s a range of responses to different opioids and doses, Warsh says. A patient who has been taking moderately high doses of opioids might be functioning well, while another patient could take a much lower dose and experience serious side effects. The London-based family doctor is confident in his ability to prescribe the right dose, duration and type of opioids, as long as he takes the time to assess the patient carefully. He is especially careful to make sure he is considering the patient’s preferences in his decision-making process.
Some of the most difficult prescribing decisions for Warsh are those for patients who have pain but also a history of problematic drug use. “One patient I can recall had a history of drug addiction, and she previously had opioids cut off because of so-called ‘red flag’ behaviours,” Warsh says. “The patient had diabetes, though, and over time developed nerve damage. No doubt about it, she was in pain. She tried all the other modalities in good faith – physiotherapy, mindfulness, and non-opioid medications – but nothing worked. What do you do? In the end I contracted with the patient to take opioids daily at the pharmacy. Over time, we found a dose that worked and let her take the medications at home because she demonstrated that she was using them as prescribed.”
Warsh says it’s more challenging when patients have multiple health conditions, past trauma, and other issues. “Maybe they shouldn’t have been prescribed opioids in the first place,” he says, “but they were, and now they are where they are.”
The Road Ahead
The overall number of new starts of opioid prescriptions in Ontario is on a slow downward trend, which could indicate that opioid prescribing practices are changing in response to new guidelines. However, there were still 1.3 million new starts in 2016, and although it is difficult to determine the ideal number of new starts, the variation by LHIN region and type of prescriber shows that there is almost certainly room for improvement. The reasons behind the LHIN variation for new starts on high doses of opioids, new starts of hydromorphone and tramadol, and new starts with a supply of more than 7 days’ worth of opioids warrant a closer look.
Many initiatives are underway in Ontario to improve the prescribing of opioids (new starts and renewals).
The Ministry of Health and Long-Term Care’s comprehensive strategy addresses opioid-related harms with a focus on three main areas:
- Modernizing opioid prescribing and monitoring
- Improving the treatment of pain
- Enhancing addictions supports and harm reduction
Health Quality Ontario’s three quality standards that are in development outline what quality care looks like for opioid prescribing for acute pain, chronic pain, and people with opioid use disorder. Developed in collaboration with patients, doctors, nurses, other health care providers, caregivers, and organizations across the province, the quality standards provide a blueprint for prescribing practices.
These standards will be leveraged into action through coordinated efforts with a number of health care organizations to provide customized data, tools and supports for appropriate prescribing.[ 21 ] This work has begun with practice reports for family doctors about their own practice relative to peers across the province, and will likely expand to include other opioid prescribers, such as surgeons, emergency department doctors, dentists, and nurse practitioners.
Many other initiatives on opioid harm reduction and pain management are underway by family doctors, surgeons and dentists. A couple of examples:
Several academic health centres in the province are developing Transitional Pain Programs, designed to help with the post-discharge period for patients who have had major surgery, and other painful medical interventions. These programs aim to better manage post-surgical pain and help patients safely reduce their opioid medications with a focus on patients newly started on opioids.
The Royal College of Dental Surgeons of Ontario has produced The Role of Opioids in the Management of Acute and Chronic Pain in Dental Practice, a guideline for dentists and dental specialists in Ontario.[22] They’re also analyzing data from the Narcotics Monitoring System over the past three years to examine the trends in prescribing of opioids by dentists in Ontario.
In the future, monitoring of opioid prescribing as it relates to the adoption of the quality standards will play a key role in preventing and reducing harms for those on opioids. The stories from the patients and doctors in this report show just how difficult it can be to achieve the right balance between pain management and preventing harm. With continued collaboration between the many groups involved, everyone needs to get it right.
Methods Notes
The Methods Notes provide a brief description of the methods used in this report.
Data sources
The analyses for this report were conducted by the Institute for Clinical Evaluative Sciences (ICES) and included data from the following administrative databases; the Narcotics Monitoring System (NMS), the Corporate Provider Database and the Registered Persons Database. Population estimates were from Statistics Canada. For more detailed descriptions about each database used, please see the Technical Appendix.
Narcotics Monitoring System, Ministry of Health and Long-Term Care
The Narcotics Monitoring System is a transaction-based system that collects dispensing data on opioids, controlled substances, and other monitored drugs from pharmacies and other dispensaries across Ontario. The information collected in the NMS includes prescriber identification, patient identification, pharmacy and pharmacist identification, date the drug was dispensed, drug identification number and the amount of drug dispensed. The NMS does not include information about monitored drugs dispensed to an in-patient of a public hospital or to prisoners or inmates (i.e., prescriptions written for people confined to correctional institutions, penitentiaries, prisons or youth custody facilities). The Ministry of Health and Long-Term Care maintains the NMS, which began collecting data in April 2012, and reporting became mandatory July 1st, 2012.
Corporate Provider Database, Ministry of Health and Long-Term Care
The Corporate Provider Database (CPDB) is a repository of healthcare provider data. The CPDB contains information on the providers’ reported specialties and postal code of practice. The Ministry of Health and Long-Term Care maintains the CPDB, with the College of Physicians and Surgeons of Ontario providing regular updates on provider credentials.
Registered Persons Database
The Registered Persons Database (RPDB) is a historical listing of the unique health numbers issued to each person eligible for Ontario health services. This listing includes corresponding demographic information, such as date of birth, sex, address, and date of death (where applicable). ICES creates an enriched postal code dataset that uses RPDB postal code data in conjunction with other administrative data holdings to generate the best known postal code on July 1st of each year for eligible individuals in the RPDB.
Population estimates, Statistics Canada
Population estimates for Ontario and LHIN regions from Statistics Canada Table 109-5355 – Estimates of population (2011 Census and administrative data). CANSIM Accessed July 2017.
Analysis
Prescribers
The report focuses on opioid dispenses and recipients among Ontario healthcare professionals who prescribed opioids to control non-palliative pain. This is a count of the number of healthcare professionals who prescribed at least one opioid drug in one of the included years (2013, 2014, 2015, 2016) excluding prescriptions that were for people who had received palliative care in the previous year, prescriptions that were to manage opioid use disorder (methadone maintenance treatment or suboxone) and prescriptions for cough medications that contain opioids. Information on the prescriber type was drawn from the NMS and from the CPDB (for physicians). In the report, we group prescribers into family physicians, surgeons, dentists and other doctors and other non-doctors (for example, the “other doctors” category includes internal medicine, psychiatry, and other physician specialties as well as doctors practising family practice and surgery but are missing these codes in the ICES data. Examples of professions included in the “other non-doctors” category includes nurses and pharmacists).
Exclusions (palliative care services, treatment of opioid use disorder, cough formulations containing opioids)
This report focuses on prescriptions for opioids that were to control non-palliative pain. As such, we excluded prescriptions that were to manage opioid use disorder, prescriptions for cough medications that contain an opioid and prescriptions that were to patients who had received palliative care. Prescriptions filled were categorized as being for palliative care if the patient had received a palliative care service in the prior 12 months either in hospital or from a physician. Prescriptions that were either for methadone for maintenance therapy or that were for naloxone/buprenorphine (suboxone) were excluded since they are for the management of opioid use disorder. Prescriptions that were for cough formulations that included an opioid were excluded since they were presumed to be for managing cough.
Opioid recipients
The report also describes the number of people in Ontario who were prescribed and dispensed at least one opioid drug to control non-palliative pain in 2013, 2014, 2015 or 2016. The total number of people prescribed an opioid is reported as well as the number of people prescribed by one of the prescriber groups. A person will be counted only once in the total provincial number for any one year. When reporting numbers of recipients by provider type, a person will be counted once for each provider group. As such, the sum of people prescribed an opioid by provider type will be greater than the provincial number. Rates per population are calculated by dividing the number of individuals who were prescribed and dispensed an opioid by the size of the population in Ontario or in the LHIN region and are reported using a 10,000 population denominator.
Opioid dispenses
The report describes the number of dispenses for opioid drugs to control non-palliative pain in 2013, 2014, 2015 or 2016. The measure was calculated as a total count as well as a count by prescriber type. The counts and rates per population were reported for Ontario and the 14 individual LHINs. Rates per population are calculated by dividing the number of dispenses for opioid drugs by the size of the population in Ontario or in the LHIN and are reported using a 10,000 population denominator.
New starts
The report describes prescriptions that were categorized as new starts for patients. For a person to be considered as newly started on an opioid, they had to have not been prescribed an opioid to manage pain in the six months prior to the prescription. The look back excluded prescriptions that were for cough medications that contained opioids or prescriptions for methadone maintenance treatment or suboxone. Patients who were identified as having received palliative care in the 12 months prior to the index prescription in a given year were also excluded. In this report, we further classified the new starts by dosage (morphine equivalents), days supplied and the type of opioid prescribed.
Days’ supply
For all new starts, the days’ supply field in the NMS estimates the number of days of treatment and was used to categorize the days supplied for a patient by a prescriber. For patients who were newly started on an opioid, if they filled prescriptions for the same opioid by the same prescriber more than one time on the same day, the days supplied for the two prescriptions were added together to calculate a total days’ supply. Days’ supply were categorized into 3 or fewer days, 4–7 days, 8–14 days or greater than 14 days supply.
Dosage (morphine equivalents)
For all new starts, the dosage or morphine equivalent (MEQ) daily dose was calculated based on the type of drug prescribed, the days supply and the quantity. For patients who were newly started on an opioid, if they filled prescriptions for the same opioid more than once or two different opioids by the same prescriber on the same day, the sum of the days’ supply and quantity were used to calculate the MEQ. MEQ was categorized into less than or equal to 50 MEQ, 51-90 MEQ or greater than 90 MEQ.
Drug type
For all new starts, the type of drug prescribed was identified using the DIN (Drug identification number) in the NMS. The opioid types included in this report were:
- Codeine
- Codeine combinations
- Fentanyl patches and tablets
- Hydromorphone
- Meperidine
- Morphine
- Oxycodone
- Oxycodone compounds
- Tramadol
- Methadone for pain
- Other
Report Development
Health Quality Ontario thanks Sara, Sheldon, Dr. Frank Warsh and Dr. Hance Clarke for sharing their experiences and insights for the quotes and stories in this report.
This report was developed by a multidisciplinary team from Health Quality Ontario, including Michael Beckett, Susan Brien, Sara Clemens, Naushaba Degani, Gail Dobell, Ryan Emond, Terri Goveia, Louise Grenier, Michal Kapral, Ryan Monte, and Binil Tahlan.
Health Quality Ontario thanks the many dedicated people who contributed to this report, including those who reviewed drafts or provided input at different stages of development: Maureen Boon, Bjug Borgundvaag, Hance Clarke, Maaike de Vries, Mario Franco Elia, Tara Gomes, Jordan Hunt, Karey Iron, David Kaplan, Mae Katt, Pamela Leece, and David Mock.
Notes: Some of the indicators in this report were derived using health administrative datasets from Ontario. These datasets were linked using unique encoded identifiers and analyzed at ICES.
ICES is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by the Institute for Clinical Evaluative Sciences or the Ontario Ministry of Health and Long-Term Care is intended or should be inferred.
References
- The Report of the International Narcotics Control Board for 2016. https://www.incb.org/documents/Narcotic-Drugs/Technical-Publications/2016/Narcotic_Drugs_Publication_2016.pdf
- The 2017 Canadian Guideline for Opioids for Chronic Non-Cancer Pain, Busse J et al. Available from: http://nationalpaincentre.mcmaster.ca/documents/Opioid%20GL%20for%20CMAJ_01may2017.pdf
- Quality standards on opioid prescribing draft recommendations http://www.hqontario.ca/Evidence-to-Improve-Care/Quality-Standards/View-all-Quality-Standards
- Barnett ML, Olenski AR, Jena AB. Opioid-Prescribing Patterns of Emergency Physicians and Risk of Long-Term Use. New England Journal of Medicine, 2017; 376:663-673. Available from: http://www.nejm.org/doi/full/10.1056/NEJMsa1610524#t=article
- Gomes T, Pasricha S, Martins D, Greaves S, et al. Behind the Prescriptions: A snapshot of opioid use across all Ontarians. Toronto: Ontario Drug Policy Research Network; August 2017.
- The 2017 Canadian Guideline for Opioids for Chronic Non-Cancer Pain, Busse J et al. Available from: http://nationalpaincentre.mcmaster.ca/documents/ Opioid%20GL%20for%20CMAJ_01may2017.pdf
- Public Health Ontario https://www.publichealthontario.ca/en/dataandanalytics/pages/opioid.aspx
- Public Health Ontario https://www.publichealthontario.ca/en/dataandanalytics/pages/opioid.aspx
- Dhalla, IA, Mamdani MM, Gomes T, Juurlink DN. Clustering of opioid prescribing and opioidrelated mortality among family physicians in Ontario. Can Fam Physician, 2011. Available from: https://www.ncbi.nlm.nih.gov/m/pubmed/21402956/?i=15&from=dhalla%20i%20
- College of Nurses in Ontario. NPs and Prescribing Controlled Substances, 2017. http://www.cno.org/en/trending-topics/nps-and-prescribingcontrolled-substances/gomes%20t
- Gomes T, Mamdani MM, Dhalla IA, Paterson J, Juurlink DN. Opioid Dose and Drug-Related Mortality in Patients With Nonmalignant Pain, Arch Intern Med. 2011;171(7):686-691
- Gomes T, Changes in the dispensing of opioid medications in Canada following the introduction of a tamper-deterrent formulation of long-acting oxycodone: a time series analysis http://cmajopen.ca/content/5/4/E800.full
- Khan S.; Government of Canada Publications Public Works and Government Services Canada. Canada Gazette Part I. July 2007.
- Globe and Mail, Nov. 22, 2017. Health Canada eyes opioid restrictions for popular painkiller https://www.theglobeandmail.com/news/national/health-canada-eyes-opioid-restrictions-forpopular-painkillertramadol/article37048483/
- 9 Million Prescriptions, Health Quality Ontario, 2017.
- Stamer UM, et al. Concentrations of Tramadol and O-desmethyltramadol Enantiomers in Different CYP2D6 Genotypes. Clinical Pharmacology and Therapeutics. Available from: http://onlinelibrary.wiley.com/doi/10.1038/sj.clpt.6100152/abstract
- Odonkor, CA, Chhatre C. What’s Tramadol Got to Do with It? A Case Report of Rebound Hypoglycemia, a Reappraisal and Review of Potential Mechanisms. Available from: http://www.painphysicianjournal.com/current/pdf?article=MzEyMg%3D%3D&journal=100
- Labate A. Tramadol and new-onset seizures https://www.mja.com.au/journal/2005/182/1/tramadol-and-new-onset-seizures
- Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain – United States, 2016. MMWR Recomm Rep. 2016;65(1):1-49.
- Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain – United States, 2016. MMWR Recomm Rep. 2016;65(1):1-49.
- http://www.hqontario.ca/Quality-Improvement/Guides-Tools-and-Practice-Reports/Primary-Care/Partnered-Supports-for-Helping-Patients-Manage-Pain
- http://www.rcdso.org/save.aspx?id=39590fd3-5eb5-46a6-991b-258bff5d0cae